Chronic Obstructive Pulmonary Disease
COPD, or chronic obstructive pulmonary (PULL-mun-ary) disease, is a progressive disease that makes it hard to breathe. "Progressive" means the disease gets worse over time.
Chronic Obstructive Pulmonary Disease (COPD) makes it hard for you to breathe. Coughing up mucus is often the first sign of COPD. Chronic bronchitis andemphysema are common COPDs.
COPD can cause coughing that produces large amounts of mucus (a slimy substance), wheezing, shortness of breath, chest tightness, and other symptoms.
Your airways branch out inside your lungs like an upside-down tree. At the end of each branch are small, balloon-like air sacs. In healthy people, both the airways and air sacs are springy and elastic. When you breathe in, each air sac fills with air like a small balloon. The balloon deflates when you exhale. In COPD, your airways and air sacs lose their shape and become floppy, like a stretched-out rubber band.
Cigarette smoking is the most common cause of COPD. Breathing in other kinds of irritants, like pollution, dust or chemicals, may also cause or contribute to COPD.Quitting smoking is the best way to avoid developing COPD.
Treatment can make you more comfortable, but there is no cure.
Overview.
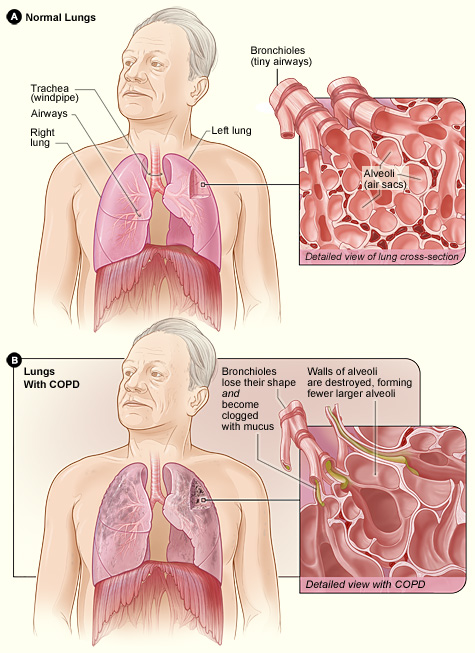
To understand COPD, it helps to understand how the lungs work. The air that you breathe goes down your windpipe into tubes in your lungs called bronchial (BRONG-ke-al) tubes or airways.
Within the lungs, your bronchial tubes branch into thousands of smaller, thinner tubes called bronchioles (BRONG-ke-ols). These tubes end in bunches of tiny round air sacs called alveoli (al-VEE-uhl-eye).
Small blood vessels called capillaries (KAP-ih-lare-ees) run through the walls of the air sacs. When air reaches the air sacs, oxygen passes through the air sac walls into the blood in the capillaries. At the same time, carbon dioxide (a waste gas) moves from the capillaries into the air sacs. This process is called gas exchange.
The airways and air sacs are elastic (stretchy). When you breathe in, each air sac fills up with air like a small balloon. When you breathe out, the air sacs deflate and the air goes out.
In COPD, less air flows in and out of the airways because of one or more of the following:
The airways and air sacs lose their elastic quality.
The walls between many of the air sacs are destroyed.
The walls of the airways become thick and inflamed.
The airways make more mucus than usual, which can clog them.
Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed cross-section of the bronchioles and alveoli. Figure B shows lungs damaged by COPD. The inset image shows a detailed cross-section of the damaged bronchioles and alveolar walls.
In the United States, the term "COPD" includes two main conditions—emphysema (em-fih-SE-ma) and chronic bronchitis (bron-KI-tis). (Note: The Health Topics article about bronchitis discusses both acute and chronic bronchitis.)
In emphysema, the walls between many of the air sacs are damaged. As a result, the air sacs lose their shape and become floppy. This damage also can destroy the walls of the air sacs, leading to fewer and larger air sacs instead of many tiny ones. If this happens, the amount of gas exchange in the lungs is reduced.
In chronic bronchitis, the lining of the airways is constantly irritated and inflamed. This causes the lining to thicken. Lots of thick mucus forms in the airways, making it hard to breathe.
Most people who have COPD have both emphysema and chronic bronchitis. Thus, the general term "COPD" is more accurate.
Outlook.
COPD is a major cause of disability, and it's the third leading cause of death in the United States. Currently, millions of people are diagnosed with COPD. Many more people may have the disease and not even know it.
COPD develops slowly. Symptoms often worsen over time and can limit your ability to do routine activities. Severe COPD may prevent you from doing even basic activities like walking, cooking, or taking care of yourself.
Most of the time, COPD is diagnosed in middle-aged or older adults. The disease isn't passed from person to person—you can't catch it from someone else.
COPD has no cure yet, and doctors don't know how to reverse the damage to the airways and lungs. However, treatments and lifestyle changes can help you feel better, stay more active, and slow the progress of the disease